15/03/2023
Published in
The Conversation
Ignacio López Goñi
Full Professor of Microbiology
March 2020. Cases of covid-19 are proliferating at an alarming rate in New York City. In the absence of footage of what is happening to covid-19 sufferers in hospitals, filmmaker Matthew Heineman decides to get into the eye of the hurricane and begins documenting the first wave of the pandemic in the Intensive Care Unit of New York's Long Island Jewish Medical Center. Thus was born The First Wavethe first documentary on the covid-19 pandemic, was born.
It is not a Hollywood movie with fictitious actors, but a real National Geographic documentary of what was experienced in New York during the first four months of the pandemic. A very hard documentary that reflects the work and the dedication of the staff health care workers, their frustration and exhaustion. It looks death in the face, its devastating trace, the desperation. The First Wave is a testament to the strength of the human spirit that captures the emotional and social impacts of the pandemic.
Lack of coordination and insufficient traceability, among other errors
During its screening as a finalist in the #LabMeCrazy scientific film festival that we organized at the Science Museum University of Navarra, the spectators remembered how, at that moment, life stopped for all of us. And still, three years later, its "side effects" continue.
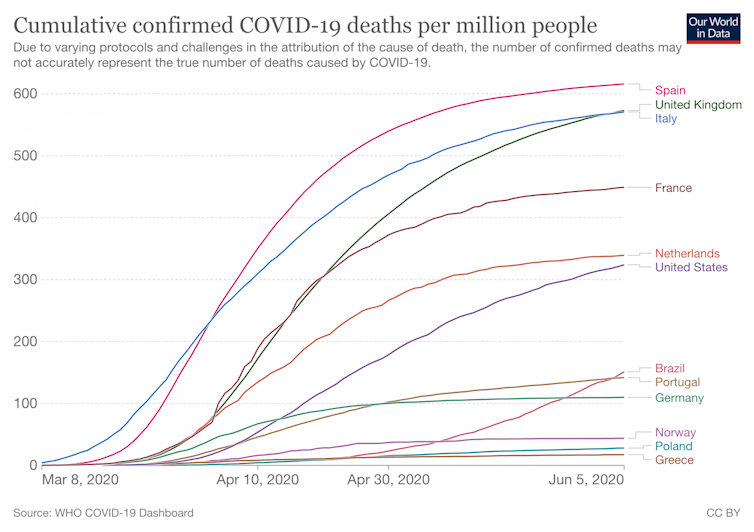
What sample The First Wave was not only experienced in New York. Moreover, if we compare the first wave (deaths in the first months) in the USA and in Spain, the difference is striking. Because Spain was, precisely, one of the countries with the highest issue of cases of deaths due to covid-19 in proportion to issue of inhabitants. For months, Spain led the issue of infected and deaths registered in Europe.
In September 2020, Juan Ignacio Perez Iglesias and I wrote a article graduate Covid-19: ten reasons to explain how we got to this point. status. Lack of leadership, lack of coordination, lack of data and the misleading role of science, political brawl, lack of pedagogy and transparency in communication, a slow crisis response followed by a hasty de-escalation, an insufficient diagnosis, tracking and isolation system and, above all, a very weakened healthcare system, led us to a great collective failure. Until the arrival of vaccines, we became one of the countries where the pandemic had the greatest impact.
Taiwan set an example
Among all the countries there was one that was spared from that first wave: the island of Taiwan. With just over 35,000 km², a population of over 23 million inhabitants, a density of 668 inhabitants/km² and only 130 km from China, Taiwan only reported fees of 0.3 deaths per million inhabitants, one of the lowest figures in the world. To put this in context, in August 2020 Belgium had fees of 861 deaths per million, and the United Kingdom of 621.
In Spain, with more than 47 million inhabitants, we have a population density of 93 inhabitants/km², seven times less than Taiwan. If we compare the issue number of deaths due to covid-19 throughout the pandemic, Taiwan has had 18 425 and Spain 119 618. This means an accumulated 800 deaths per million in Taiwan compared to 2 545 in Spain.
What did Taiwan do to resist that first wave?
Most surprisingly, it did not carry out strict containment as we did in Europe. Taiwan was simply prepared for a pandemic because it had already experienced the SARS pandemic threat in 2003.
It announced its first case of covid-19 on January 21, 2020: a 50-year-old woman returning to Taiwan from the city of Wuhan. The response of the authorities was immediate and forceful, starting with a diagnostic test of all passengers coming from Wuhan.
As of mid-March, restrictions were added to entrance on foreigners entering the country, quarantine (14 days at home) and control of all citizens coming from high-risk countries, distribution and use of masks among the population, as well as a ban on meetings of more than 100 people indoors and more than 500 outdoors.
As in other Asian countries, in Taiwan, the culture of mask use in public (social acceptance) had already existed since 2004 and there was universal access to masks. In addition, there was a national health agency capable of effectively coordinating decision making and preventing and controlling this subject emergency situations, with forcefulness and speed, and without legal impediments. They also had a digital rapid access system to identify and isolate cases.
At final, a rapid and coordinated response based on case detection, control of entrance in the country, effective isolation and quarantine methods, digital technologies to identify possible cases and massive use of masks.
And all without the need for confinement or restriction of movement within the country. This has allowed them to overcome the pandemic without devastating economic effects and without other collateral effects such as the deterioration in the mental health of citizens.
We have not yet learned from the pandemic
It is surprising to think that three years ago we went out to the balconies to applaud and pay tribute to our healthcare workers and now they are the ones who are demonstrating all over Spain to apply for financial aid . It is outrageous that none of our leaders (national and regional) have tackled a reform and improvement of the healthcare system.
This we write in September 2020:
Cuts after the 2008 crisis weakened the healthcare system. During the state of alarm, the focus was on hospital beds and ICUs. But the deficits of staff care have been obvious. It is therefore necessary to reinforce the staff of the staff healthcare system. It is essential to focus and act now on public health and primary care in order to reduce the issue of people who have to be hospitalized.
Special attention should also be paid to pediatric and geriatric services. All this implies the need to incorporate more staff and to do so as soon as possible. A healthcare system stretched to the limit has consequences that go far beyond the COVID-19 itself: delays in other diagnoses and treatments, altered child vaccination schedules, etc., with the consequent loss of health and lives.
This is perhaps the most important thing: to strengthen the health system, because this is where our lives are at stake.
